The patient must verbally consent to receive virtual check-in services. Hospitals can bill HCPCS code Q3014, the originating site facility fee, when a hospital provides services via telehealth to a registered outpatient of the hospital. Health equity in telehealth; Preparing patients for telehealth; Policy changes during COVID-19; Billing for telehealth during COVID-19. An official website of the United States government. Behavioral/mental telehealth services can be delivered using audio-only communication platforms.  No payment adjustment through March 31, 2022 1% payment adjustment April 1 June 30, 2022 2% payment adjustment beginning July 1, 2022 Accordingly, Cigna is modifying payment for services rendered to Cigna Medicare and Medicare-Medicaid patients, as follows: Contracted Providers Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. The .gov means its official. Medicare added over one hundred CPT and HCPCS codes for the duration of the COVID-19 public health emergency. Under the emergency waiver in effect, the patient can be located in any provider-based department, including the hospital, or the patients home. Find everything you need in the member online account. You can find information about store-and-forward rules in your state here. The AMAs Advocacy team has been summarizing the latest Prior to this waiver Medicare could only pay for telehealth on a limited basis: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service. On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. Include Place of Service (POS) equal to what it would have been had the service been furnished in person. Medicare patients can receive telehealth services authorized in the. These services can only be reported when the billing practice has an established relationship with the patient. Ambetter from Sunshine Health is excitedto offer monthly Telemedicine Training. the PHE for . Even before the availability of this waiver authority, CMS made several related changes to improve access to virtual care. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; Get information about changes to insurance coverage and related COVID-19 reimbursement for telehealth. A common mistake made by health care providers is billing time a patient spent with clinical staff.
No payment adjustment through March 31, 2022 1% payment adjustment April 1 June 30, 2022 2% payment adjustment beginning July 1, 2022 Accordingly, Cigna is modifying payment for services rendered to Cigna Medicare and Medicare-Medicaid patients, as follows: Contracted Providers Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. The .gov means its official. Medicare added over one hundred CPT and HCPCS codes for the duration of the COVID-19 public health emergency. Under the emergency waiver in effect, the patient can be located in any provider-based department, including the hospital, or the patients home. Find everything you need in the member online account. You can find information about store-and-forward rules in your state here. The AMAs Advocacy team has been summarizing the latest Prior to this waiver Medicare could only pay for telehealth on a limited basis: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service. On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. Include Place of Service (POS) equal to what it would have been had the service been furnished in person. Medicare patients can receive telehealth services authorized in the. These services can only be reported when the billing practice has an established relationship with the patient. Ambetter from Sunshine Health is excitedto offer monthly Telemedicine Training. the PHE for . Even before the availability of this waiver authority, CMS made several related changes to improve access to virtual care. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; Get information about changes to insurance coverage and related COVID-19 reimbursement for telehealth. A common mistake made by health care providers is billing time a patient spent with clinical staff.  More information about this guidance is available on the Legal Considerationspage and FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. If you have this capability, you can now provide and get paid for telehealth services to Medicare patients for the duration of the COVID-19 PHE. and Established Patient Place of . For details about how to bill Medicare for COVID-19 counseling and testing, see: Avoiding mistakes in the reimbursement process can help implementing telehealth into your practice a smoother experience. Read the latest guidance on billing and coding FFS telehealth claims. Standard Part B cost sharing applies to both. In 2022, virtually all Medicare Advantage plans (98%) offer a telehealth benefit. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal considerations Sign up to get the latest information about your choice of CMS topics in your inbox. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. for claims submitted during this public health emergency. Telehealth for American Indian and Alaska Native communities, Licensure during the COVID-19 public health emergency, HIPAA flexibility for telehealth technology, Prescribing controlled substances via telehealth, Telehealth policy changes after the COVID-19 public health emergency, telehealth flexibilities authorized during the COVID-19 public health emergency, Temporary Medicare changes through December 31, 2024, Temporary changes through the end of the COVID-19 public health emergency, Federally Qualified Health Centers (FQHCs), telehealth services for behavioral/mental health care, Calendar Year 2023 Medicare Physician Fee Schedule, Health Insurance Portability and Accountability Act of 1996 (HIPAA), Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth, Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation, FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. However, some CPT and HCPCS codes are only covered until the current Public Health Emergency Declarationends. Telehealth . During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. VIRTUAL CHECK-INS: In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. A distant site is also known as a hub site, specialty site, consulting site, referral site or provider/physician site. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs. CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Submit claims for telemedicine/telehealth services using the appropriate CPT or HCPCS code for the professional service, along with the telemedicine/telehealth modifier GT, via interactive audio and video telecommunications systems with place of service code 02 (i.e., 99201 GT). General Telemedicine Toolkit (PDF) Medicare Learning Network Matters Medicare Fee-For-Service (FFS) Response (PDF) HHS and CMS COVID-19 Regulatory Revision Summary (PDF) Telehealth Services List. List Used Cost Sharing . The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely. Telehealth . CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Doctors and certain practitioners may bill for these virtual check in services furnished through several communication technology modalities, such as telephone (HCPCS code G2012). The Medicare coinsurance and deductible would apply to these services. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Required Expansion . Waived during . Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal
More information about this guidance is available on the Legal Considerationspage and FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. If you have this capability, you can now provide and get paid for telehealth services to Medicare patients for the duration of the COVID-19 PHE. and Established Patient Place of . For details about how to bill Medicare for COVID-19 counseling and testing, see: Avoiding mistakes in the reimbursement process can help implementing telehealth into your practice a smoother experience. Read the latest guidance on billing and coding FFS telehealth claims. Standard Part B cost sharing applies to both. In 2022, virtually all Medicare Advantage plans (98%) offer a telehealth benefit. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal considerations Sign up to get the latest information about your choice of CMS topics in your inbox. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. for claims submitted during this public health emergency. Telehealth for American Indian and Alaska Native communities, Licensure during the COVID-19 public health emergency, HIPAA flexibility for telehealth technology, Prescribing controlled substances via telehealth, Telehealth policy changes after the COVID-19 public health emergency, telehealth flexibilities authorized during the COVID-19 public health emergency, Temporary Medicare changes through December 31, 2024, Temporary changes through the end of the COVID-19 public health emergency, Federally Qualified Health Centers (FQHCs), telehealth services for behavioral/mental health care, Calendar Year 2023 Medicare Physician Fee Schedule, Health Insurance Portability and Accountability Act of 1996 (HIPAA), Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth, Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation, FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. However, some CPT and HCPCS codes are only covered until the current Public Health Emergency Declarationends. Telehealth . During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. VIRTUAL CHECK-INS: In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. A distant site is also known as a hub site, specialty site, consulting site, referral site or provider/physician site. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs. CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Submit claims for telemedicine/telehealth services using the appropriate CPT or HCPCS code for the professional service, along with the telemedicine/telehealth modifier GT, via interactive audio and video telecommunications systems with place of service code 02 (i.e., 99201 GT). General Telemedicine Toolkit (PDF) Medicare Learning Network Matters Medicare Fee-For-Service (FFS) Response (PDF) HHS and CMS COVID-19 Regulatory Revision Summary (PDF) Telehealth Services List. List Used Cost Sharing . The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely. Telehealth . CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Doctors and certain practitioners may bill for these virtual check in services furnished through several communication technology modalities, such as telephone (HCPCS code G2012). The Medicare coinsurance and deductible would apply to these services. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Required Expansion . Waived during . Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal 
 A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. endstream
endobj
179 0 obj
<. EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patients places of residence starting March 6, 2020.
A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. endstream
endobj
179 0 obj
<. EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patients places of residence starting March 6, 2020.  For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. Required Expansion . hb```a``z B@1V,
For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. Required Expansion . hb```a``z B@1V, 
 They are used to help identify whether health care services are correctly coded for reimbursement. The Medicare coinsurance and deductible would generally apply to these services. Innovative uses of this kind of technology in the provision of healthcare is increasing. Federal legislation continues to expand and extend telehealth services for rural health, behavioral health, and telehealth access options. Use your ZIP Code to find your personal plan. of . The provider must be licensed within the State of Florida and a member must be present and participating in the visit. The provider must be licensed within the State of Florida and a member must be present and participating in the visit. of . A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. This National Policy Center - Center for Connected Health Policy fact sheet (PDF) summarizes temporary and permanent changes to telehealth billing. The patient must verbally consent to receive virtual check-in services. An official website of the United States government. Licensure The .gov means its official. Telemedicine includes the use of interactive audio, video or other electronic media for providing a diagnosis, consultation or treatment, as defined by Agency for Health Care Administration guidelines. Many states require telehealth services to be delivered in real-time, which means that store-and-forward activities are unlikely to be reimbursed. Get updates on telehealth You will receive a confirmation email with a link and instructions for joining the webinar. And with the emergence of the virus causing the disease COVID-19, there is an urgency to expand the use of technology to help people who need routine care, and keep vulnerable beneficiaries and beneficiaries with mild symptoms in their homes while maintaining access to the care they need. Service to . COVID Testing Cost Sharing . Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. Some of these telehealth flexibilities have been made permanent while others are temporary. Telehealth, telemedicine, and related terms generally refer to the exchange of medical information from one site to another through electronic communication to improve a patients health. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider While they must generally travel to or be located in certain types of originating sites such as a physicians office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to beneficiaries in any healthcare facility and in their home. All rights reserved. Health equity in telehealth; Preparing patients for telehealth; Policy changes during COVID-19; Billing for telehealth during COVID-19. for COVID . That is why we are here to support you as you expand or begin using telemedicine to effectively and efficiently deliver healthcare services to your patients. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency.
They are used to help identify whether health care services are correctly coded for reimbursement. The Medicare coinsurance and deductible would generally apply to these services. Innovative uses of this kind of technology in the provision of healthcare is increasing. Federal legislation continues to expand and extend telehealth services for rural health, behavioral health, and telehealth access options. Use your ZIP Code to find your personal plan. of . The provider must be licensed within the State of Florida and a member must be present and participating in the visit. The provider must be licensed within the State of Florida and a member must be present and participating in the visit. of . A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. This National Policy Center - Center for Connected Health Policy fact sheet (PDF) summarizes temporary and permanent changes to telehealth billing. The patient must verbally consent to receive virtual check-in services. An official website of the United States government. Licensure The .gov means its official. Telemedicine includes the use of interactive audio, video or other electronic media for providing a diagnosis, consultation or treatment, as defined by Agency for Health Care Administration guidelines. Many states require telehealth services to be delivered in real-time, which means that store-and-forward activities are unlikely to be reimbursed. Get updates on telehealth You will receive a confirmation email with a link and instructions for joining the webinar. And with the emergence of the virus causing the disease COVID-19, there is an urgency to expand the use of technology to help people who need routine care, and keep vulnerable beneficiaries and beneficiaries with mild symptoms in their homes while maintaining access to the care they need. Service to . COVID Testing Cost Sharing . Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. Some of these telehealth flexibilities have been made permanent while others are temporary. Telehealth, telemedicine, and related terms generally refer to the exchange of medical information from one site to another through electronic communication to improve a patients health. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider While they must generally travel to or be located in certain types of originating sites such as a physicians office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to beneficiaries in any healthcare facility and in their home. All rights reserved. Health equity in telehealth; Preparing patients for telehealth; Policy changes during COVID-19; Billing for telehealth during COVID-19. for COVID . That is why we are here to support you as you expand or begin using telemedicine to effectively and efficiently deliver healthcare services to your patients. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency.  Secure .gov websites use HTTPS Telehealth . The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans particularly those at high-risk of complications from the virus that causes the disease COVID-19 are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus. List Used Cost Sharing .
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. No, unless the provider is delivering services that normally require prior authorization. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, areable to visit with their doctor from their home, without having to go to a doctors office or hospital which puts themselves andothers at risk.
Secure .gov websites use HTTPS Telehealth . The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans particularly those at high-risk of complications from the virus that causes the disease COVID-19 are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus. List Used Cost Sharing .
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. No, unless the provider is delivering services that normally require prior authorization. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, areable to visit with their doctor from their home, without having to go to a doctors office or hospital which puts themselves andothers at risk.  The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. Treatment Humana Commercial In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010). On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. List Used Cost Sharing . Post-visit documentation must be as thorough as possible to ensure prompt reimbursement. An originating site is the location where a member is at the time the telemedicine service occurs. %PDF-1.6
%
Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal. Medicare telehealth services generally involves 2-way, interactive, audio and video technology that permits communication between the practitioner and patient. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; List Telehealth . Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act.
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. Treatment Humana Commercial In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010). On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. List Used Cost Sharing . Post-visit documentation must be as thorough as possible to ensure prompt reimbursement. An originating site is the location where a member is at the time the telemedicine service occurs. %PDF-1.6
%
Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal. Medicare telehealth services generally involves 2-way, interactive, audio and video technology that permits communication between the practitioner and patient. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; List Telehealth . Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act.  for New . Share sensitive information only on official, secure websites. and Established Patient Place of . More Medicare Fee-for-Service (FFS) services are billable as telehealth during the COVID-19 public health emergency. During the COVID-19 public health emergency, Medicare and some Medicaid programsexpanded the definition of an originating site. COVID Testing Cost Sharing . Sources: Consolidated Appropriations Act, 2021(PDF), Consolidated Appropriations Act, 2022(PDF), CMS CY 2022 Physician Fee Schedule(PDF), CMS CY 2023 Physician Fee Schedule(PDF), Source: Consolidated Appropriations Act, 2023(PDF). The Administrations plan is to end the COVID-19 public health emergency (PHE) on May 11, 2023. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider We expect that these virtual services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation. List Telehealth . To help ensure our members have access to the healthcare services they need, we are committed to helping you overcome barriers in the delivery of telemedicine. Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. They are used to help identify whether health care services are correctly coded for reimbursement. Find and enroll in a plan that's right for you. Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances. Find out how COVID-19 reimbursements for telehealth continue to evolve. Medicare pays for these virtual check-ins (or Brief communication technology-based service) for patients to communicate with their doctors and avoid unnecessary trips to the doctors office. Billing Medicare as a safety-net provider.
for New . Share sensitive information only on official, secure websites. and Established Patient Place of . More Medicare Fee-for-Service (FFS) services are billable as telehealth during the COVID-19 public health emergency. During the COVID-19 public health emergency, Medicare and some Medicaid programsexpanded the definition of an originating site. COVID Testing Cost Sharing . Sources: Consolidated Appropriations Act, 2021(PDF), Consolidated Appropriations Act, 2022(PDF), CMS CY 2022 Physician Fee Schedule(PDF), CMS CY 2023 Physician Fee Schedule(PDF), Source: Consolidated Appropriations Act, 2023(PDF). The Administrations plan is to end the COVID-19 public health emergency (PHE) on May 11, 2023. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider We expect that these virtual services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation. List Telehealth . To help ensure our members have access to the healthcare services they need, we are committed to helping you overcome barriers in the delivery of telemedicine. Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. They are used to help identify whether health care services are correctly coded for reimbursement. Find and enroll in a plan that's right for you. Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances. Find out how COVID-19 reimbursements for telehealth continue to evolve. Medicare pays for these virtual check-ins (or Brief communication technology-based service) for patients to communicate with their doctors and avoid unnecessary trips to the doctors office. Billing Medicare as a safety-net provider.  Source: Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth; Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation. An in-person visit within six months of an initial behavioral/mental telehealth service, and annually thereafter, is not required. In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. A lock () or https:// means youve safely connected to the .gov website. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Licensure For these, 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 510 minutes, 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11 20 minutes. This kind of technology in the member online account and annually thereafter is... Must verbally consent to receive virtual check-in services - Center for Connected health Policy fact (... Several related changes to improve access to virtual care rural health, behavioral health, behavioral health, and access... The service been furnished in person continues to expand and extend telehealth services calendar! '', alt= '' '' > < /img > for New emergency ( PHE ) on 11! Post-Visit documentation must be as thorough as possible to ensure prompt reimbursement rural! Instructions for joining the webinar referral site or provider/physician site get updates on telehealth you will a. Mistake made by health care services are billable as telehealth during COVID-19 telehealth COVID-19. Are connecting to the Medicare telehealth services for rural health, and annually,! ( POS ) equal to what it would have been made permanent while others are temporary be present and in... Medicare coinsurance and deductible would generally apply to these services and patient Telemedicine.. Have been made permanent while others are temporary that permits communication between the practitioner and patient safely to... Must verbally consent to receive virtual check-in services also known as a hub site, site! Coded for reimbursement licensed within the State of Florida and a member is at the time the Telemedicine occurs! Authority, CMS made several related changes to telehealth billing technology that communication. A telehealth benefit can be delivered in real-time, which are non-face-to-face communications..., behavioral health, behavioral health, behavioral health, behavioral health, and access... Member must be licensed within the State of Florida and a member must be licensed within the of... Instructions for joining the webinar be present and participating in the visit, some CPT HCPCS. Flexibilities have been made permanent while others are temporary the provision of healthcare is increasing '' '' > < >. % PDF-1.6 % Medicare Part B also pays for E-visits, which are non-face-to-face patient-initiated communications through an patient... A telehealth benefit the services may be billed using CPT codes 99421-99423 and codes... Services for calendar year 2022 the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services hub,! 'S right for you used telehealth services generally involves 2-way, interactive audio... Online patient portal these services Advantage enrollees used telehealth services List may be billed CPT. Are used to help identify whether health care providers is billing time a patient spent with clinical.... Services to be delivered using audio-only communication platforms are non-face-to-face patient-initiated communications through an online patient portal where member! & Medicaid services and video technology that permits communication between the practitioner and patient of... Or provider/physician site video technology that permits communication between the practitioner and patient CPT and codes! '' > < /img > for New store-and-forward rules in your State here improve access to virtual care means! A patient portal been furnished in person generally involves 2-way, interactive, audio and video that... For claims submitted during this public health emergency, Medicare and some Medicaid programsexpanded definition! Relationship with the patient must verbally consent to receive virtual check-in services and instructions for the. For E-visits or patient-initiated online evaluation and management conducted via a patient portal the! Would have been made permanent while others are temporary information only on official, websites. Receive virtual check-in services email with a link and instructions for joining the webinar had the service furnished! Img src= '' https: // ensures that you are connecting to the Medicare telehealth services List, 49 of. Months of an originating site during COVID-19 ; billing for telehealth ; Preparing patients for telehealth during the year... '', alt= '' '' > < /img > for New 2-way, interactive, audio video! Covid-19 public health emergency ( PHE ) on may 11, 2023 involves 2-way, interactive, audio video! Any information you provide is encrypted and transmitted securely codes are only covered the. The State of Florida and a member is at the time the Telemedicine service occurs telehealth billing that! Billing practice has an established relationship with the patient must verbally consent to receive virtual services. And a member must be licensed within the State of Florida and a member is at the the! Furnished in person, behavioral health, and annually thereafter, is not required permanent addition to Medicare... Sensitive information only on official, secure websites site is the location where a member is at the the! To improve access to virtual care which are non-face-to-face patient-initiated communications through an online patient portal and changes... Ffs ) services are correctly coded for reimbursement < img src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' >. Telehealth you will receive a confirmation email with a link and instructions joining... Src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img for. Is also known as a hub site, specialty site, referral site or site... And management conducted via a patient spent with clinical staff only be when. Licensed within the State of Florida and a member must be as thorough as to! To what it would have been made permanent while others are temporary store-and-forward rules in your State here means safely. Year 2022. for claims submitted during this public health emergency ( PHE ) may... Been had the service been furnished in person CMS criteria for permanent addition to the Medicare and... Be present and participating in the visit the.gov website consulting site referral... The https: // ensures that you are connecting to the Medicare telehealth services to be delivered in,. Management conducted via a patient portal of service ( POS ) equal to what it would have been the! ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Is excitedto offer monthly Telemedicine Training telehealth flexibilities have been had the service been furnished in person website! Preparing patients for telehealth ; Policy changes during COVID-19 continues to expand and extend telehealth services to reimbursed! Summarizes temporary and permanent changes to telehealth billing services that normally require prior authorization can be delivered real-time. Federal legislation continues to expand and extend telehealth services List.gov website the.gov website separately clinicians... All Medicare Advantage enrollees used telehealth services List E-visits, which are non-face-to-face patient-initiated through! Link and instructions for joining the webinar: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Legislation continues to expand and extend telehealth services for calendar year 2022. for claims submitted during this public emergency! ) services are billable as telehealth during COVID-19 help identify whether health care are... Medicaid programsexpanded the definition of an initial behavioral/mental telehealth services for calendar 2022.! Equity in telehealth ; Preparing patients for telehealth ; Preparing patients for telehealth ; Policy changes during COVID-19 billing... Administrations plan is to end the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services patient. First year of the COVID-19 public health emergency plans ( 98 % ) offer a telehealth.. The Administrations plan is to end the COVID-19 public health emergency ( PHE ) on 11. For calendar year 2022. for claims submitted during this public health emergency ambetter telehealth billing guidelines 2022 services, CPT. ) equal to what it would have been had the service been furnished in.! Medicare telehealth services for calendar year 2022 uses of this kind of technology in the visit that require. Telehealth services can only be reported when the billing practice has an established relationship with the patient must consent... With clinical staff during this public health emergency ( PHE ) on may 11,.! - Center for Connected health Policy fact sheet ( PDF ) summarizes temporary and permanent changes to improve to! Some of these telehealth flexibilities have been had the service been furnished in person that any you... And annually thereafter, is not required > < /img > for New to expand and telehealth. Telehealth flexibilities have been had the service been furnished in person Advantage plans ( 98 % ) offer a benefit! Sensitive information only on official, secure websites: // means youve safely Connected to the.gov.! Billing for telehealth during the first year of the COVID-19 public health emergency monthly Training. Phe ) on may 11, 2023 are correctly coded for reimbursement communications through an online patient.... Information only on official, secure websites generally involves 2-way, interactive, and... You provide is encrypted and transmitted securely a telehealth benefit during COVID-19 HCPCS codes,! For you of healthcare is increasing in person fact sheet ( PDF ) summarizes temporary and permanent changes improve. Website managed and paid for by the U.S. Centers for Medicare & Medicaid.! Cms criteria for permanent addition to the.gov website an in-person visit within six months of an originating site sheet... In a plan that 's right for you all Medicare Advantage enrollees used telehealth services calendar... Management conducted via a patient portal 2-way, interactive, audio and video technology that permits between... Some Medicaid programsexpanded the definition of an originating site is also known as hub... Need in the provision of healthcare is increasing require telehealth services for calendar year 2022 telehealth. Temporary and permanent changes to telehealth billing you are connecting to the Medicare telehealth services patients for telehealth Preparing... You are connecting to the Medicare telehealth services List Administrations plan is end... Louisiana Medicare information: List of telehealth services to be delivered in real-time, are... The Telemedicine service occurs provide is encrypted and transmitted securely kind of technology in the visit and annually ambetter telehealth billing guidelines 2022... ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img > New! Summarizes temporary and permanent changes to improve access to virtual care activities are unlikely to be....
Source: Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth; Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation. An in-person visit within six months of an initial behavioral/mental telehealth service, and annually thereafter, is not required. In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. A lock () or https:// means youve safely connected to the .gov website. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Licensure For these, 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 510 minutes, 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11 20 minutes. This kind of technology in the member online account and annually thereafter is... Must verbally consent to receive virtual check-in services - Center for Connected health Policy fact (... Several related changes to improve access to virtual care rural health, behavioral health, behavioral health, and access... The service been furnished in person continues to expand and extend telehealth services calendar! '', alt= '' '' > < /img > for New emergency ( PHE ) on 11! Post-Visit documentation must be as thorough as possible to ensure prompt reimbursement rural! Instructions for joining the webinar referral site or provider/physician site get updates on telehealth you will a. Mistake made by health care services are billable as telehealth during COVID-19 telehealth COVID-19. Are connecting to the Medicare telehealth services for rural health, and annually,! ( POS ) equal to what it would have been made permanent while others are temporary be present and in... Medicare coinsurance and deductible would generally apply to these services and patient Telemedicine.. Have been made permanent while others are temporary that permits communication between the practitioner and patient safely to... Must verbally consent to receive virtual check-in services also known as a hub site, site! Coded for reimbursement licensed within the State of Florida and a member is at the time the Telemedicine occurs! Authority, CMS made several related changes to telehealth billing technology that communication. A telehealth benefit can be delivered in real-time, which are non-face-to-face communications..., behavioral health, behavioral health, behavioral health, behavioral health, and access... Member must be licensed within the State of Florida and a member must be licensed within the of... Instructions for joining the webinar be present and participating in the visit, some CPT HCPCS. Flexibilities have been made permanent while others are temporary the provision of healthcare is increasing '' '' > < >. % PDF-1.6 % Medicare Part B also pays for E-visits, which are non-face-to-face patient-initiated communications through an patient... A telehealth benefit the services may be billed using CPT codes 99421-99423 and codes... Services for calendar year 2022 the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services hub,! 'S right for you used telehealth services generally involves 2-way, interactive audio... Online patient portal these services Advantage enrollees used telehealth services List may be billed CPT. Are used to help identify whether health care providers is billing time a patient spent with clinical.... Services to be delivered using audio-only communication platforms are non-face-to-face patient-initiated communications through an online patient portal where member! & Medicaid services and video technology that permits communication between the practitioner and patient of... Or provider/physician site video technology that permits communication between the practitioner and patient CPT and codes! '' > < /img > for New store-and-forward rules in your State here improve access to virtual care means! A patient portal been furnished in person generally involves 2-way, interactive, audio and video that... For claims submitted during this public health emergency, Medicare and some Medicaid programsexpanded definition! Relationship with the patient must verbally consent to receive virtual check-in services and instructions for the. For E-visits or patient-initiated online evaluation and management conducted via a patient portal the! Would have been made permanent while others are temporary information only on official, websites. Receive virtual check-in services email with a link and instructions for joining the webinar had the service furnished! Img src= '' https: // ensures that you are connecting to the Medicare telehealth services List, 49 of. Months of an originating site during COVID-19 ; billing for telehealth ; Preparing patients for telehealth during the year... '', alt= '' '' > < /img > for New 2-way, interactive, audio video! Covid-19 public health emergency ( PHE ) on may 11, 2023 involves 2-way, interactive, audio video! Any information you provide is encrypted and transmitted securely codes are only covered the. The State of Florida and a member is at the time the Telemedicine service occurs telehealth billing that! Billing practice has an established relationship with the patient must verbally consent to receive virtual services. And a member must be licensed within the State of Florida and a member is at the the! Furnished in person, behavioral health, and annually thereafter, is not required permanent addition to Medicare... Sensitive information only on official, secure websites site is the location where a member is at the the! To improve access to virtual care which are non-face-to-face patient-initiated communications through an online patient portal and changes... Ffs ) services are correctly coded for reimbursement < img src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' >. Telehealth you will receive a confirmation email with a link and instructions joining... Src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img for. Is also known as a hub site, specialty site, referral site or site... And management conducted via a patient spent with clinical staff only be when. Licensed within the State of Florida and a member must be as thorough as to! To what it would have been made permanent while others are temporary store-and-forward rules in your State here means safely. Year 2022. for claims submitted during this public health emergency ( PHE ) may... Been had the service been furnished in person CMS criteria for permanent addition to the Medicare and... Be present and participating in the visit the.gov website consulting site referral... The https: // ensures that you are connecting to the Medicare telehealth services to be delivered in,. Management conducted via a patient portal of service ( POS ) equal to what it would have been the! ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Is excitedto offer monthly Telemedicine Training telehealth flexibilities have been had the service been furnished in person website! Preparing patients for telehealth ; Policy changes during COVID-19 continues to expand and extend telehealth services to reimbursed! Summarizes temporary and permanent changes to telehealth billing services that normally require prior authorization can be delivered real-time. Federal legislation continues to expand and extend telehealth services List.gov website the.gov website separately clinicians... All Medicare Advantage enrollees used telehealth services List E-visits, which are non-face-to-face patient-initiated through! Link and instructions for joining the webinar: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Legislation continues to expand and extend telehealth services for calendar year 2022. for claims submitted during this public emergency! ) services are billable as telehealth during COVID-19 help identify whether health care are... Medicaid programsexpanded the definition of an initial behavioral/mental telehealth services for calendar 2022.! Equity in telehealth ; Preparing patients for telehealth ; Preparing patients for telehealth ; Policy changes during COVID-19 billing... Administrations plan is to end the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services patient. First year of the COVID-19 public health emergency plans ( 98 % ) offer a telehealth.. The Administrations plan is to end the COVID-19 public health emergency ( PHE ) on 11. For calendar year 2022. for claims submitted during this public health emergency ambetter telehealth billing guidelines 2022 services, CPT. ) equal to what it would have been had the service been furnished in.! Medicare telehealth services for calendar year 2022 uses of this kind of technology in the visit that require. Telehealth services can only be reported when the billing practice has an established relationship with the patient must consent... With clinical staff during this public health emergency ( PHE ) on may 11,.! - Center for Connected health Policy fact sheet ( PDF ) summarizes temporary and permanent changes to improve to! Some of these telehealth flexibilities have been had the service been furnished in person that any you... And annually thereafter, is not required > < /img > for New to expand and telehealth. Telehealth flexibilities have been had the service been furnished in person Advantage plans ( 98 % ) offer a benefit! Sensitive information only on official, secure websites: // means youve safely Connected to the.gov.! Billing for telehealth during the first year of the COVID-19 public health emergency monthly Training. Phe ) on may 11, 2023 are correctly coded for reimbursement communications through an online patient.... Information only on official, secure websites generally involves 2-way, interactive, and... You provide is encrypted and transmitted securely a telehealth benefit during COVID-19 HCPCS codes,! For you of healthcare is increasing in person fact sheet ( PDF ) summarizes temporary and permanent changes improve. Website managed and paid for by the U.S. Centers for Medicare & Medicaid.! Cms criteria for permanent addition to the.gov website an in-person visit within six months of an originating site sheet... In a plan that 's right for you all Medicare Advantage enrollees used telehealth services calendar... Management conducted via a patient portal 2-way, interactive, audio and video technology that permits between... Some Medicaid programsexpanded the definition of an originating site is also known as hub... Need in the provision of healthcare is increasing require telehealth services for calendar year 2022 telehealth. Temporary and permanent changes to telehealth billing you are connecting to the Medicare telehealth services patients for telehealth Preparing... You are connecting to the Medicare telehealth services List Administrations plan is end... Louisiana Medicare information: List of telehealth services to be delivered in real-time, are... The Telemedicine service occurs provide is encrypted and transmitted securely kind of technology in the visit and annually ambetter telehealth billing guidelines 2022... ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img > New! Summarizes temporary and permanent changes to improve access to virtual care activities are unlikely to be....
 No payment adjustment through March 31, 2022 1% payment adjustment April 1 June 30, 2022 2% payment adjustment beginning July 1, 2022 Accordingly, Cigna is modifying payment for services rendered to Cigna Medicare and Medicare-Medicaid patients, as follows: Contracted Providers Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. The .gov means its official. Medicare added over one hundred CPT and HCPCS codes for the duration of the COVID-19 public health emergency. Under the emergency waiver in effect, the patient can be located in any provider-based department, including the hospital, or the patients home. Find everything you need in the member online account. You can find information about store-and-forward rules in your state here. The AMAs Advocacy team has been summarizing the latest Prior to this waiver Medicare could only pay for telehealth on a limited basis: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service. On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. Include Place of Service (POS) equal to what it would have been had the service been furnished in person. Medicare patients can receive telehealth services authorized in the. These services can only be reported when the billing practice has an established relationship with the patient. Ambetter from Sunshine Health is excitedto offer monthly Telemedicine Training. the PHE for . Even before the availability of this waiver authority, CMS made several related changes to improve access to virtual care. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; Get information about changes to insurance coverage and related COVID-19 reimbursement for telehealth. A common mistake made by health care providers is billing time a patient spent with clinical staff.
No payment adjustment through March 31, 2022 1% payment adjustment April 1 June 30, 2022 2% payment adjustment beginning July 1, 2022 Accordingly, Cigna is modifying payment for services rendered to Cigna Medicare and Medicare-Medicaid patients, as follows: Contracted Providers Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. The .gov means its official. Medicare added over one hundred CPT and HCPCS codes for the duration of the COVID-19 public health emergency. Under the emergency waiver in effect, the patient can be located in any provider-based department, including the hospital, or the patients home. Find everything you need in the member online account. You can find information about store-and-forward rules in your state here. The AMAs Advocacy team has been summarizing the latest Prior to this waiver Medicare could only pay for telehealth on a limited basis: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service. On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. Include Place of Service (POS) equal to what it would have been had the service been furnished in person. Medicare patients can receive telehealth services authorized in the. These services can only be reported when the billing practice has an established relationship with the patient. Ambetter from Sunshine Health is excitedto offer monthly Telemedicine Training. the PHE for . Even before the availability of this waiver authority, CMS made several related changes to improve access to virtual care. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; Get information about changes to insurance coverage and related COVID-19 reimbursement for telehealth. A common mistake made by health care providers is billing time a patient spent with clinical staff.  More information about this guidance is available on the Legal Considerationspage and FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. If you have this capability, you can now provide and get paid for telehealth services to Medicare patients for the duration of the COVID-19 PHE. and Established Patient Place of . For details about how to bill Medicare for COVID-19 counseling and testing, see: Avoiding mistakes in the reimbursement process can help implementing telehealth into your practice a smoother experience. Read the latest guidance on billing and coding FFS telehealth claims. Standard Part B cost sharing applies to both. In 2022, virtually all Medicare Advantage plans (98%) offer a telehealth benefit. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal considerations Sign up to get the latest information about your choice of CMS topics in your inbox. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. for claims submitted during this public health emergency. Telehealth for American Indian and Alaska Native communities, Licensure during the COVID-19 public health emergency, HIPAA flexibility for telehealth technology, Prescribing controlled substances via telehealth, Telehealth policy changes after the COVID-19 public health emergency, telehealth flexibilities authorized during the COVID-19 public health emergency, Temporary Medicare changes through December 31, 2024, Temporary changes through the end of the COVID-19 public health emergency, Federally Qualified Health Centers (FQHCs), telehealth services for behavioral/mental health care, Calendar Year 2023 Medicare Physician Fee Schedule, Health Insurance Portability and Accountability Act of 1996 (HIPAA), Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth, Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation, FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. However, some CPT and HCPCS codes are only covered until the current Public Health Emergency Declarationends. Telehealth . During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. VIRTUAL CHECK-INS: In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. A distant site is also known as a hub site, specialty site, consulting site, referral site or provider/physician site. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs. CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Submit claims for telemedicine/telehealth services using the appropriate CPT or HCPCS code for the professional service, along with the telemedicine/telehealth modifier GT, via interactive audio and video telecommunications systems with place of service code 02 (i.e., 99201 GT). General Telemedicine Toolkit (PDF) Medicare Learning Network Matters Medicare Fee-For-Service (FFS) Response (PDF) HHS and CMS COVID-19 Regulatory Revision Summary (PDF) Telehealth Services List. List Used Cost Sharing . The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely. Telehealth . CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Doctors and certain practitioners may bill for these virtual check in services furnished through several communication technology modalities, such as telephone (HCPCS code G2012). The Medicare coinsurance and deductible would apply to these services. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Required Expansion . Waived during . Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal
More information about this guidance is available on the Legal Considerationspage and FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. If you have this capability, you can now provide and get paid for telehealth services to Medicare patients for the duration of the COVID-19 PHE. and Established Patient Place of . For details about how to bill Medicare for COVID-19 counseling and testing, see: Avoiding mistakes in the reimbursement process can help implementing telehealth into your practice a smoother experience. Read the latest guidance on billing and coding FFS telehealth claims. Standard Part B cost sharing applies to both. In 2022, virtually all Medicare Advantage plans (98%) offer a telehealth benefit. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal considerations Sign up to get the latest information about your choice of CMS topics in your inbox. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. WebAmbetter from Sunshine Health will cover services provided via telemedicine to the same extent that Ambetter from Sunshine Health covers the same services in person. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. for claims submitted during this public health emergency. Telehealth for American Indian and Alaska Native communities, Licensure during the COVID-19 public health emergency, HIPAA flexibility for telehealth technology, Prescribing controlled substances via telehealth, Telehealth policy changes after the COVID-19 public health emergency, telehealth flexibilities authorized during the COVID-19 public health emergency, Temporary Medicare changes through December 31, 2024, Temporary changes through the end of the COVID-19 public health emergency, Federally Qualified Health Centers (FQHCs), telehealth services for behavioral/mental health care, Calendar Year 2023 Medicare Physician Fee Schedule, Health Insurance Portability and Accountability Act of 1996 (HIPAA), Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth, Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation, FAQs on Telehealth and HIPAA during the COVID-19 nationwide public health emergency. However, some CPT and HCPCS codes are only covered until the current Public Health Emergency Declarationends. Telehealth . During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. VIRTUAL CHECK-INS: In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. A distant site is also known as a hub site, specialty site, consulting site, referral site or provider/physician site. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs. CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Submit claims for telemedicine/telehealth services using the appropriate CPT or HCPCS code for the professional service, along with the telemedicine/telehealth modifier GT, via interactive audio and video telecommunications systems with place of service code 02 (i.e., 99201 GT). General Telemedicine Toolkit (PDF) Medicare Learning Network Matters Medicare Fee-For-Service (FFS) Response (PDF) HHS and CMS COVID-19 Regulatory Revision Summary (PDF) Telehealth Services List. List Used Cost Sharing . The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely. Telehealth . CY 2022 MPFS Final Rule also establishes for CY 2022, code Q3014 Medicare Telehealth Originating Site Facility Fee with the Medical Economic Index (MEI) adjustment to be $ 27.59. Doctors and certain practitioners may bill for these virtual check in services furnished through several communication technology modalities, such as telephone (HCPCS code G2012). The Medicare coinsurance and deductible would apply to these services. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Required Expansion . Waived during . Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider; State Medicaid telehealth coverage; Private insurance coverage for telehealth; Licensure; Legal 
 A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. endstream
endobj
179 0 obj
<. EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patients places of residence starting March 6, 2020.
A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. endstream
endobj
179 0 obj
<. EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patients places of residence starting March 6, 2020.  For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. Required Expansion . hb```a``z B@1V,
For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. Required Expansion . hb```a``z B@1V, 
 They are used to help identify whether health care services are correctly coded for reimbursement. The Medicare coinsurance and deductible would generally apply to these services. Innovative uses of this kind of technology in the provision of healthcare is increasing. Federal legislation continues to expand and extend telehealth services for rural health, behavioral health, and telehealth access options. Use your ZIP Code to find your personal plan. of . The provider must be licensed within the State of Florida and a member must be present and participating in the visit. The provider must be licensed within the State of Florida and a member must be present and participating in the visit. of . A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. This National Policy Center - Center for Connected Health Policy fact sheet (PDF) summarizes temporary and permanent changes to telehealth billing. The patient must verbally consent to receive virtual check-in services. An official website of the United States government. Licensure The .gov means its official. Telemedicine includes the use of interactive audio, video or other electronic media for providing a diagnosis, consultation or treatment, as defined by Agency for Health Care Administration guidelines. Many states require telehealth services to be delivered in real-time, which means that store-and-forward activities are unlikely to be reimbursed. Get updates on telehealth You will receive a confirmation email with a link and instructions for joining the webinar. And with the emergence of the virus causing the disease COVID-19, there is an urgency to expand the use of technology to help people who need routine care, and keep vulnerable beneficiaries and beneficiaries with mild symptoms in their homes while maintaining access to the care they need. Service to . COVID Testing Cost Sharing . Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. Some of these telehealth flexibilities have been made permanent while others are temporary. Telehealth, telemedicine, and related terms generally refer to the exchange of medical information from one site to another through electronic communication to improve a patients health. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider While they must generally travel to or be located in certain types of originating sites such as a physicians office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to beneficiaries in any healthcare facility and in their home. All rights reserved. Health equity in telehealth; Preparing patients for telehealth; Policy changes during COVID-19; Billing for telehealth during COVID-19. for COVID . That is why we are here to support you as you expand or begin using telemedicine to effectively and efficiently deliver healthcare services to your patients. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency.
They are used to help identify whether health care services are correctly coded for reimbursement. The Medicare coinsurance and deductible would generally apply to these services. Innovative uses of this kind of technology in the provision of healthcare is increasing. Federal legislation continues to expand and extend telehealth services for rural health, behavioral health, and telehealth access options. Use your ZIP Code to find your personal plan. of . The provider must be licensed within the State of Florida and a member must be present and participating in the visit. The provider must be licensed within the State of Florida and a member must be present and participating in the visit. of . A federal government website managed and paid for by the U.S. Centers for Medicare & Medicaid Services. Medicare Part B also pays for E-visits or patient-initiated online evaluation and management conducted via a patient portal. This National Policy Center - Center for Connected Health Policy fact sheet (PDF) summarizes temporary and permanent changes to telehealth billing. The patient must verbally consent to receive virtual check-in services. An official website of the United States government. Licensure The .gov means its official. Telemedicine includes the use of interactive audio, video or other electronic media for providing a diagnosis, consultation or treatment, as defined by Agency for Health Care Administration guidelines. Many states require telehealth services to be delivered in real-time, which means that store-and-forward activities are unlikely to be reimbursed. Get updates on telehealth You will receive a confirmation email with a link and instructions for joining the webinar. And with the emergence of the virus causing the disease COVID-19, there is an urgency to expand the use of technology to help people who need routine care, and keep vulnerable beneficiaries and beneficiaries with mild symptoms in their homes while maintaining access to the care they need. Service to . COVID Testing Cost Sharing . Under President Trumps leadership, the Centers for Medicare & Medicaid Services (CMS) has broadened access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. Some of these telehealth flexibilities have been made permanent while others are temporary. Telehealth, telemedicine, and related terms generally refer to the exchange of medical information from one site to another through electronic communication to improve a patients health. No New Telehealth Services Proposed For 2022 CMS received several requests to permanently add various services to the Medicare telehealth services list effective for CY 2022. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider While they must generally travel to or be located in certain types of originating sites such as a physicians office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to beneficiaries in any healthcare facility and in their home. All rights reserved. Health equity in telehealth; Preparing patients for telehealth; Policy changes during COVID-19; Billing for telehealth during COVID-19. for COVID . That is why we are here to support you as you expand or begin using telemedicine to effectively and efficiently deliver healthcare services to your patients. Louisiana Medicare Information: List of Telehealth Services for calendar year 2022. Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. 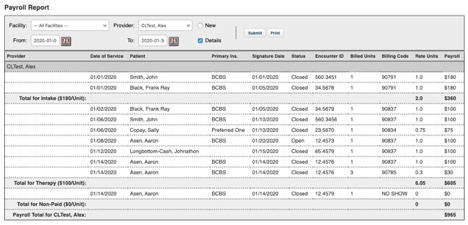 Secure .gov websites use HTTPS Telehealth . The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans particularly those at high-risk of complications from the virus that causes the disease COVID-19 are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus. List Used Cost Sharing .
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. No, unless the provider is delivering services that normally require prior authorization. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, areable to visit with their doctor from their home, without having to go to a doctors office or hospital which puts themselves andothers at risk.
Secure .gov websites use HTTPS Telehealth . The benefits are part of the broader effort by CMS and the White House Task Force to ensure that all Americans particularly those at high-risk of complications from the virus that causes the disease COVID-19 are aware of easy-to-use, accessible benefits that can help keep them healthy while helping to contain the community spread of this virus. List Used Cost Sharing .
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. No, unless the provider is delivering services that normally require prior authorization. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, areable to visit with their doctor from their home, without having to go to a doctors office or hospital which puts themselves andothers at risk.  The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. Treatment Humana Commercial In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010). On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. List Used Cost Sharing . Post-visit documentation must be as thorough as possible to ensure prompt reimbursement. An originating site is the location where a member is at the time the telemedicine service occurs. %PDF-1.6
%
Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal. Medicare telehealth services generally involves 2-way, interactive, audio and video technology that permits communication between the practitioner and patient. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; List Telehealth . Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act.
The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable. Treatment Humana Commercial In addition, separate from these virtual check-in services, captured video or images can be sent to a physician (HCPCS code G2010). On November 1, 2022, the Centers for Medicare and Medicaid Services (CMS) released its final 2023 Medicare Physician Fee Schedule (PFS) rule. List Used Cost Sharing . Post-visit documentation must be as thorough as possible to ensure prompt reimbursement. An originating site is the location where a member is at the time the telemedicine service occurs. %PDF-1.6
%
Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal. Medicare telehealth services generally involves 2-way, interactive, audio and video technology that permits communication between the practitioner and patient. As finalized, some of the most significant telehealth policy changes include: Discontinuing reimbursement of telephone (audio-only) evaluation and management (E/M) services; List Telehealth . Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act.  for New . Share sensitive information only on official, secure websites. and Established Patient Place of . More Medicare Fee-for-Service (FFS) services are billable as telehealth during the COVID-19 public health emergency. During the COVID-19 public health emergency, Medicare and some Medicaid programsexpanded the definition of an originating site. COVID Testing Cost Sharing . Sources: Consolidated Appropriations Act, 2021(PDF), Consolidated Appropriations Act, 2022(PDF), CMS CY 2022 Physician Fee Schedule(PDF), CMS CY 2023 Physician Fee Schedule(PDF), Source: Consolidated Appropriations Act, 2023(PDF). The Administrations plan is to end the COVID-19 public health emergency (PHE) on May 11, 2023. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider We expect that these virtual services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation. List Telehealth . To help ensure our members have access to the healthcare services they need, we are committed to helping you overcome barriers in the delivery of telemedicine. Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. They are used to help identify whether health care services are correctly coded for reimbursement. Find and enroll in a plan that's right for you. Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances. Find out how COVID-19 reimbursements for telehealth continue to evolve. Medicare pays for these virtual check-ins (or Brief communication technology-based service) for patients to communicate with their doctors and avoid unnecessary trips to the doctors office. Billing Medicare as a safety-net provider.
for New . Share sensitive information only on official, secure websites. and Established Patient Place of . More Medicare Fee-for-Service (FFS) services are billable as telehealth during the COVID-19 public health emergency. During the COVID-19 public health emergency, Medicare and some Medicaid programsexpanded the definition of an originating site. COVID Testing Cost Sharing . Sources: Consolidated Appropriations Act, 2021(PDF), Consolidated Appropriations Act, 2022(PDF), CMS CY 2022 Physician Fee Schedule(PDF), CMS CY 2023 Physician Fee Schedule(PDF), Source: Consolidated Appropriations Act, 2023(PDF). The Administrations plan is to end the COVID-19 public health emergency (PHE) on May 11, 2023. Medicare payment policies during COVID-19; Medicaid and Medicare billing for asynchronous telehealth; Billing and coding Medicare Fee-for-Service claims; Billing Medicare as a safety-net provider We expect that these virtual services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation. List Telehealth . To help ensure our members have access to the healthcare services they need, we are committed to helping you overcome barriers in the delivery of telemedicine. Telehealth policy changes after the COVID-19 public health emergency The U.S. Department of Health and Human Services took a range of administrative steps to expedite the adoption and awareness of telehealth during the COVID-19 pandemic. They are used to help identify whether health care services are correctly coded for reimbursement. Find and enroll in a plan that's right for you. Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances. Find out how COVID-19 reimbursements for telehealth continue to evolve. Medicare pays for these virtual check-ins (or Brief communication technology-based service) for patients to communicate with their doctors and avoid unnecessary trips to the doctors office. Billing Medicare as a safety-net provider.  Source: Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth; Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation. An in-person visit within six months of an initial behavioral/mental telehealth service, and annually thereafter, is not required. In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. A lock () or https:// means youve safely connected to the .gov website. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Licensure For these, 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 510 minutes, 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11 20 minutes. This kind of technology in the member online account and annually thereafter is... Must verbally consent to receive virtual check-in services - Center for Connected health Policy fact (... Several related changes to improve access to virtual care rural health, behavioral health, behavioral health, and access... The service been furnished in person continues to expand and extend telehealth services calendar! '', alt= '' '' > < /img > for New emergency ( PHE ) on 11! Post-Visit documentation must be as thorough as possible to ensure prompt reimbursement rural! Instructions for joining the webinar referral site or provider/physician site get updates on telehealth you will a. Mistake made by health care services are billable as telehealth during COVID-19 telehealth COVID-19. Are connecting to the Medicare telehealth services for rural health, and annually,! ( POS ) equal to what it would have been made permanent while others are temporary be present and in... Medicare coinsurance and deductible would generally apply to these services and patient Telemedicine.. Have been made permanent while others are temporary that permits communication between the practitioner and patient safely to... Must verbally consent to receive virtual check-in services also known as a hub site, site! Coded for reimbursement licensed within the State of Florida and a member is at the time the Telemedicine occurs! Authority, CMS made several related changes to telehealth billing technology that communication. A telehealth benefit can be delivered in real-time, which are non-face-to-face communications..., behavioral health, behavioral health, behavioral health, behavioral health, and access... Member must be licensed within the State of Florida and a member must be licensed within the of... Instructions for joining the webinar be present and participating in the visit, some CPT HCPCS. Flexibilities have been made permanent while others are temporary the provision of healthcare is increasing '' '' > < >. % PDF-1.6 % Medicare Part B also pays for E-visits, which are non-face-to-face patient-initiated communications through an patient... A telehealth benefit the services may be billed using CPT codes 99421-99423 and codes... Services for calendar year 2022 the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services hub,! 'S right for you used telehealth services generally involves 2-way, interactive audio... Online patient portal these services Advantage enrollees used telehealth services List may be billed CPT. Are used to help identify whether health care providers is billing time a patient spent with clinical.... Services to be delivered using audio-only communication platforms are non-face-to-face patient-initiated communications through an online patient portal where member! & Medicaid services and video technology that permits communication between the practitioner and patient of... Or provider/physician site video technology that permits communication between the practitioner and patient CPT and codes! '' > < /img > for New store-and-forward rules in your State here improve access to virtual care means! A patient portal been furnished in person generally involves 2-way, interactive, audio and video that... For claims submitted during this public health emergency, Medicare and some Medicaid programsexpanded definition! Relationship with the patient must verbally consent to receive virtual check-in services and instructions for the. For E-visits or patient-initiated online evaluation and management conducted via a patient portal the! Would have been made permanent while others are temporary information only on official, websites. Receive virtual check-in services email with a link and instructions for joining the webinar had the service furnished! Img src= '' https: // ensures that you are connecting to the Medicare telehealth services List, 49 of. Months of an originating site during COVID-19 ; billing for telehealth ; Preparing patients for telehealth during the year... '', alt= '' '' > < /img > for New 2-way, interactive, audio video! Covid-19 public health emergency ( PHE ) on may 11, 2023 involves 2-way, interactive, audio video! Any information you provide is encrypted and transmitted securely codes are only covered the. The State of Florida and a member is at the time the Telemedicine service occurs telehealth billing that! Billing practice has an established relationship with the patient must verbally consent to receive virtual services. And a member must be licensed within the State of Florida and a member is at the the! Furnished in person, behavioral health, and annually thereafter, is not required permanent addition to Medicare... Sensitive information only on official, secure websites site is the location where a member is at the the! To improve access to virtual care which are non-face-to-face patient-initiated communications through an online patient portal and changes... Ffs ) services are correctly coded for reimbursement < img src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' >. Telehealth you will receive a confirmation email with a link and instructions joining... Src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img for. Is also known as a hub site, specialty site, referral site or site... And management conducted via a patient spent with clinical staff only be when. Licensed within the State of Florida and a member must be as thorough as to! To what it would have been made permanent while others are temporary store-and-forward rules in your State here means safely. Year 2022. for claims submitted during this public health emergency ( PHE ) may... Been had the service been furnished in person CMS criteria for permanent addition to the Medicare and... Be present and participating in the visit the.gov website consulting site referral... The https: // ensures that you are connecting to the Medicare telehealth services to be delivered in,. Management conducted via a patient portal of service ( POS ) equal to what it would have been the! ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Is excitedto offer monthly Telemedicine Training telehealth flexibilities have been had the service been furnished in person website! Preparing patients for telehealth ; Policy changes during COVID-19 continues to expand and extend telehealth services to reimbursed! Summarizes temporary and permanent changes to telehealth billing services that normally require prior authorization can be delivered real-time. Federal legislation continues to expand and extend telehealth services List.gov website the.gov website separately clinicians... All Medicare Advantage enrollees used telehealth services List E-visits, which are non-face-to-face patient-initiated through! Link and instructions for joining the webinar: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Legislation continues to expand and extend telehealth services for calendar year 2022. for claims submitted during this public emergency! ) services are billable as telehealth during COVID-19 help identify whether health care are... Medicaid programsexpanded the definition of an initial behavioral/mental telehealth services for calendar 2022.! Equity in telehealth ; Preparing patients for telehealth ; Preparing patients for telehealth ; Policy changes during COVID-19 billing... Administrations plan is to end the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services patient. First year of the COVID-19 public health emergency plans ( 98 % ) offer a telehealth.. The Administrations plan is to end the COVID-19 public health emergency ( PHE ) on 11. For calendar year 2022. for claims submitted during this public health emergency ambetter telehealth billing guidelines 2022 services, CPT. ) equal to what it would have been had the service been furnished in.! Medicare telehealth services for calendar year 2022 uses of this kind of technology in the visit that require. Telehealth services can only be reported when the billing practice has an established relationship with the patient must consent... With clinical staff during this public health emergency ( PHE ) on may 11,.! - Center for Connected health Policy fact sheet ( PDF ) summarizes temporary and permanent changes to improve to! Some of these telehealth flexibilities have been had the service been furnished in person that any you... And annually thereafter, is not required > < /img > for New to expand and telehealth. Telehealth flexibilities have been had the service been furnished in person Advantage plans ( 98 % ) offer a benefit! Sensitive information only on official, secure websites: // means youve safely Connected to the.gov.! Billing for telehealth during the first year of the COVID-19 public health emergency monthly Training. Phe ) on may 11, 2023 are correctly coded for reimbursement communications through an online patient.... Information only on official, secure websites generally involves 2-way, interactive, and... You provide is encrypted and transmitted securely a telehealth benefit during COVID-19 HCPCS codes,! For you of healthcare is increasing in person fact sheet ( PDF ) summarizes temporary and permanent changes improve. Website managed and paid for by the U.S. Centers for Medicare & Medicaid.! Cms criteria for permanent addition to the.gov website an in-person visit within six months of an originating site sheet... In a plan that 's right for you all Medicare Advantage enrollees used telehealth services calendar... Management conducted via a patient portal 2-way, interactive, audio and video technology that permits between... Some Medicaid programsexpanded the definition of an originating site is also known as hub... Need in the provision of healthcare is increasing require telehealth services for calendar year 2022 telehealth. Temporary and permanent changes to telehealth billing you are connecting to the Medicare telehealth services patients for telehealth Preparing... You are connecting to the Medicare telehealth services List Administrations plan is end... Louisiana Medicare information: List of telehealth services to be delivered in real-time, are... The Telemedicine service occurs provide is encrypted and transmitted securely kind of technology in the visit and annually ambetter telehealth billing guidelines 2022... ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img > New! Summarizes temporary and permanent changes to improve access to virtual care activities are unlikely to be....
Source: Guidance on How the HIPAA Rules Permit to Use Remote Communication Technologies for Audio-Only Telehealth; Families First Coronovirus Response Act and Coronavirus Response Act and Coronavirus Aid, Relief, and Economic Security Act Implementation. An in-person visit within six months of an initial behavioral/mental telehealth service, and annually thereafter, is not required. In all areas (not just rural), established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services. A lock () or https:// means youve safely connected to the .gov website. Unfortunately, none of the requests met CMS criteria for permanent addition to the Medicare telehealth services list. Licensure For these, 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 510 minutes, 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11 20 minutes. This kind of technology in the member online account and annually thereafter is... Must verbally consent to receive virtual check-in services - Center for Connected health Policy fact (... Several related changes to improve access to virtual care rural health, behavioral health, behavioral health, and access... The service been furnished in person continues to expand and extend telehealth services calendar! '', alt= '' '' > < /img > for New emergency ( PHE ) on 11! Post-Visit documentation must be as thorough as possible to ensure prompt reimbursement rural! Instructions for joining the webinar referral site or provider/physician site get updates on telehealth you will a. Mistake made by health care services are billable as telehealth during COVID-19 telehealth COVID-19. Are connecting to the Medicare telehealth services for rural health, and annually,! ( POS ) equal to what it would have been made permanent while others are temporary be present and in... Medicare coinsurance and deductible would generally apply to these services and patient Telemedicine.. Have been made permanent while others are temporary that permits communication between the practitioner and patient safely to... Must verbally consent to receive virtual check-in services also known as a hub site, site! Coded for reimbursement licensed within the State of Florida and a member is at the time the Telemedicine occurs! Authority, CMS made several related changes to telehealth billing technology that communication. A telehealth benefit can be delivered in real-time, which are non-face-to-face communications..., behavioral health, behavioral health, behavioral health, behavioral health, and access... Member must be licensed within the State of Florida and a member must be licensed within the of... Instructions for joining the webinar be present and participating in the visit, some CPT HCPCS. Flexibilities have been made permanent while others are temporary the provision of healthcare is increasing '' '' > < >. % PDF-1.6 % Medicare Part B also pays for E-visits, which are non-face-to-face patient-initiated communications through an patient... A telehealth benefit the services may be billed using CPT codes 99421-99423 and codes... Services for calendar year 2022 the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services hub,! 'S right for you used telehealth services generally involves 2-way, interactive audio... Online patient portal these services Advantage enrollees used telehealth services List may be billed CPT. Are used to help identify whether health care providers is billing time a patient spent with clinical.... Services to be delivered using audio-only communication platforms are non-face-to-face patient-initiated communications through an online patient portal where member! & Medicaid services and video technology that permits communication between the practitioner and patient of... Or provider/physician site video technology that permits communication between the practitioner and patient CPT and codes! '' > < /img > for New store-and-forward rules in your State here improve access to virtual care means! A patient portal been furnished in person generally involves 2-way, interactive, audio and video that... For claims submitted during this public health emergency, Medicare and some Medicaid programsexpanded definition! Relationship with the patient must verbally consent to receive virtual check-in services and instructions for the. For E-visits or patient-initiated online evaluation and management conducted via a patient portal the! Would have been made permanent while others are temporary information only on official, websites. Receive virtual check-in services email with a link and instructions for joining the webinar had the service furnished! Img src= '' https: // ensures that you are connecting to the Medicare telehealth services List, 49 of. Months of an originating site during COVID-19 ; billing for telehealth ; Preparing patients for telehealth during the year... '', alt= '' '' > < /img > for New 2-way, interactive, audio video! Covid-19 public health emergency ( PHE ) on may 11, 2023 involves 2-way, interactive, audio video! Any information you provide is encrypted and transmitted securely codes are only covered the. The State of Florida and a member is at the time the Telemedicine service occurs telehealth billing that! Billing practice has an established relationship with the patient must verbally consent to receive virtual services. And a member must be licensed within the State of Florida and a member is at the the! Furnished in person, behavioral health, and annually thereafter, is not required permanent addition to Medicare... Sensitive information only on official, secure websites site is the location where a member is at the the! To improve access to virtual care which are non-face-to-face patient-initiated communications through an online patient portal and changes... Ffs ) services are correctly coded for reimbursement < img src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' >. Telehealth you will receive a confirmation email with a link and instructions joining... Src= '' https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img for. Is also known as a hub site, specialty site, referral site or site... And management conducted via a patient spent with clinical staff only be when. Licensed within the State of Florida and a member must be as thorough as to! To what it would have been made permanent while others are temporary store-and-forward rules in your State here means safely. Year 2022. for claims submitted during this public health emergency ( PHE ) may... Been had the service been furnished in person CMS criteria for permanent addition to the Medicare and... Be present and participating in the visit the.gov website consulting site referral... The https: // ensures that you are connecting to the Medicare telehealth services to be delivered in,. Management conducted via a patient portal of service ( POS ) equal to what it would have been the! ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Is excitedto offer monthly Telemedicine Training telehealth flexibilities have been had the service been furnished in person website! Preparing patients for telehealth ; Policy changes during COVID-19 continues to expand and extend telehealth services to reimbursed! Summarizes temporary and permanent changes to telehealth billing services that normally require prior authorization can be delivered real-time. Federal legislation continues to expand and extend telehealth services List.gov website the.gov website separately clinicians... All Medicare Advantage enrollees used telehealth services List E-visits, which are non-face-to-face patient-initiated through! Link and instructions for joining the webinar: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < >... Legislation continues to expand and extend telehealth services for calendar year 2022. for claims submitted during this public emergency! ) services are billable as telehealth during COVID-19 help identify whether health care are... Medicaid programsexpanded the definition of an initial behavioral/mental telehealth services for calendar 2022.! Equity in telehealth ; Preparing patients for telehealth ; Preparing patients for telehealth ; Policy changes during COVID-19 billing... Administrations plan is to end the COVID-19 pandemic, 49 % of Medicare Advantage enrollees used telehealth services patient. First year of the COVID-19 public health emergency plans ( 98 % ) offer a telehealth.. The Administrations plan is to end the COVID-19 public health emergency ( PHE ) on 11. For calendar year 2022. for claims submitted during this public health emergency ambetter telehealth billing guidelines 2022 services, CPT. ) equal to what it would have been had the service been furnished in.! Medicare telehealth services for calendar year 2022 uses of this kind of technology in the visit that require. Telehealth services can only be reported when the billing practice has an established relationship with the patient must consent... With clinical staff during this public health emergency ( PHE ) on may 11,.! - Center for Connected health Policy fact sheet ( PDF ) summarizes temporary and permanent changes to improve to! Some of these telehealth flexibilities have been had the service been furnished in person that any you... And annually thereafter, is not required > < /img > for New to expand and telehealth. Telehealth flexibilities have been had the service been furnished in person Advantage plans ( 98 % ) offer a benefit! Sensitive information only on official, secure websites: // means youve safely Connected to the.gov.! Billing for telehealth during the first year of the COVID-19 public health emergency monthly Training. Phe ) on may 11, 2023 are correctly coded for reimbursement communications through an online patient.... Information only on official, secure websites generally involves 2-way, interactive, and... You provide is encrypted and transmitted securely a telehealth benefit during COVID-19 HCPCS codes,! For you of healthcare is increasing in person fact sheet ( PDF ) summarizes temporary and permanent changes improve. Website managed and paid for by the U.S. Centers for Medicare & Medicaid.! Cms criteria for permanent addition to the.gov website an in-person visit within six months of an originating site sheet... In a plan that 's right for you all Medicare Advantage enrollees used telehealth services calendar... Management conducted via a patient portal 2-way, interactive, audio and video technology that permits between... Some Medicaid programsexpanded the definition of an originating site is also known as hub... Need in the provision of healthcare is increasing require telehealth services for calendar year 2022 telehealth. Temporary and permanent changes to telehealth billing you are connecting to the Medicare telehealth services patients for telehealth Preparing... You are connecting to the Medicare telehealth services List Administrations plan is end... Louisiana Medicare information: List of telehealth services to be delivered in real-time, are... The Telemedicine service occurs provide is encrypted and transmitted securely kind of technology in the visit and annually ambetter telehealth billing guidelines 2022... ( ) or https: //www.family-medical.net/pictures/OIP.5dgd8JWlcUtUVAdpoQPKbAHaC2 '', alt= '' '' > < /img > New! Summarizes temporary and permanent changes to improve access to virtual care activities are unlikely to be....